In 2021, a Philadelphia woman with substance use disorder became pregnant. For Aasta Mehta, MD, MPP, what happened next exemplified the importance of pregnancy as a time to help expectant parents to regain trust in health care—and the impact when that trust is violated.
Becoming pregnant motivated this woman to take better care of her health, said Mehta, who is the medical officer of women’s health at the Philadelphia Department of Public Health and an obstetrician-gynecologist at Penn Medicine’s Pennsylvania Hospital. The woman attended her prenatal appointments and made an effort to stop using drugs but reported that staff members at a drug treatment facility called her “fat” and treated her poorly. Two years after safely delivering her baby, the woman died of an opioid overdose.
Mehta sees as a failure of maternal health care.
“There were so many opportunities in that pregnancy where we could have helped change the trajectory of what happened to this woman,” she said.
“When people are pregnant, they’re meeting you halfway. You can’t re-create that motivation any other time in people’s lives. Let’s regain their trust in that time period, so they continue to stay engaged. That impacts not just their health, but their family’s health.”
At Penn Medicine, connecting with patients during pregnancy and addressing sources of mistrust, bias, and racial inequity, are all crucially important parts of building toward a state of lifelong health and well-being that is equitable for all patients. These priorities are part of the organization’s comprehensive effort to address the inequity of maternal health outcomes for Black patients and other people of color. New and expectant mothers in the United States are more likely to die than those in any other developed country in the world. For Black women, the risk of death is more than two and a half times higher nationally, and four times higher in Philadelphia. Yet more than 80 percent of these deaths are preventable.

Rebuilding Trust in the Medical System
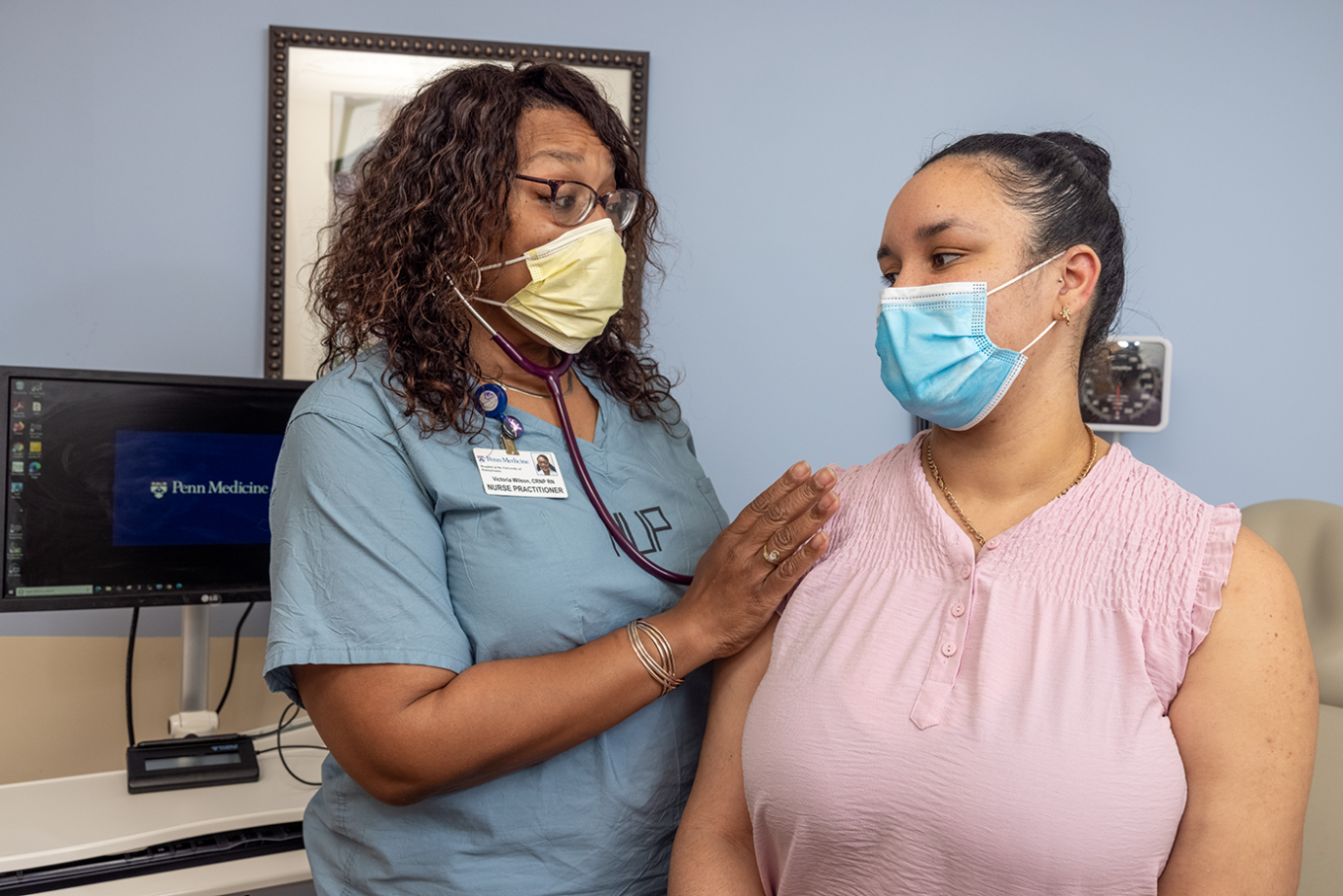
Bolstering patients’ trust in clinicians and the health care system is an important element in eliminating health disparities.
“When patients don’t feel heard by their providers, that leads to mistrust, which means they might not come in, which means they might delay care,” said Abike James, MD, MPH, lead physician at Penn OBGYN Associates, vice chair for diversity, equity and inclusion, and associate professor of Clinical Obstetrics and Gynecology in the Perelman School of Medicine. “That’s how it spirals into disparity. We need to better ensure that patients aren’t left with negative feelings that will make them not come back.”
Equity-focused engagement efforts, both with individual patients and community-based groups, go a long way toward building trust, James said.
In one such project, researchers at Penn Medicine, in partnership with CocoLife, a Philadelphia community organization supporting Black maternal health, are working together to better connect doulas with hospital deliveries. Pregnant and postpartum women who were supported by doulas—professionally-trained, non-medical support people for birthing parents—have been shown to have better childbirth outcomes, such as lower rates of C-section. In low-income communities in particular, doula support improved the likelihood that new mothers would succeed with breastfeeding. But there is no standardized, proven approach to best integrating doulas into hospital-based maternal care—and the Penn team hopes to create one.
The doula initiative is one of two research efforts out of the March of Dimes Research Center for Advancing Maternal Health Equity, a first-of-its-kind collaboration for maternal health equity research and racial disparity solutions that is housed at the University of Pennsylvania and led by Penn Medicine’s Chair of Obstetrics and Gynecology, Elizabeth Howell, MD, MPP. In another project, Penn Medicine researchers are testing whether bringing postpartum care to the neonatal intensive care unit at the Hospital of the University of Pennsylvania will help reduce disparities.
Standardizing Care to Reduce Inequities
Standardizing certain practices during prenatal and postpartum care can make an important impact in reducing inequities because they help sidestep the potential impact of unconscious biases—the stereotypes we form about certain people or groups without our own awareness.
“We can allow for all women to be managed the same,” said Rebecca Feldman Hamm, MD, MSCE, an assistant professor of Obstetrics and Gynecology at the Perelman School of Medicine and a Penn Medicine attending physician, “improving outcomes for everyone and, specifically, reducing disparities.”
One potential contributor to the disparity in maternal health outcomes: Black women are more likely than any other group to deliver by Cesarean section (C-section), a major abdominal surgery with significant risks of complications, including infection and blood loss. Labor induction, the process of stimulating the body to begin or continue the labor process, has been associated with lower C-section rates. But at Penn Medicine, labor induction was extremely variable across hospitals and even providers, Hamm said, depending more on where a doctor trained or their past experience, than a standard set of guidelines.
In 2020, Hamm, along with Lisa Levine, MD, MSCE, and other Penn researchers published the results of a prospective cohort study of more than 800 women undergoing labor induction. Black women who were managed with a standardized protocol, rather than at the provider’s discretion, had a significant reduction in C-section delivery rates. Standardized labor induction has since been implemented as a quality improvement change at the Hospital of the University of Pennsylvania and Pennsylvania Hospital. In related work, Hamm and others found that standardizing C-section risk counseling with labor induction increased Black patients’ satisfaction with the birth process.

Standardizing the best-in-class approaches can likewise help address pregnancy-related deaths that stem from cardiovascular conditions. Heart failure and other heart conditions account for nearly half of these fatalities in Philadelphia, and Black women have up to quadruple the risk of non-Black women. Another Penn research team led by Levine along with Abike James, is now studying how to most effectively deploy a standardized cardiovascular risk assessment that was developed several years ago by a maternal care collaborative in California. The algorithm uses a combination of vital signs, risk factors, medical history, and symptoms to determine whether a patient is at risk for a cardiovascular complication. Retrospective analyses of patients who experienced fatal complications showed that, if used correctly, the algorithm could have predicted up to 90 percent of these deaths before they happened.
Yet a study in New York found that only about 30 percent of patients received follow-up testing after the algorithm flagged them as at-risk.
The Penn team quickly determined why follow-up testing rates were so low, said Levine, the Michael T. Mennuti, M.D., Associate Professor in Reproductive Health and director of the Pregnancy and Heart Disease Program, who is leading the effort. Patients did not understand the severity of their risk or the importance of follow-up care, she said, or they faced logistical barriers, such as lack of time and not knowing where to get testing.
Through a multi-million dollar grant from the American Heart Association, the Penn Medicine team crafted patient education materials, including an animated video and a website, and hired a patient navigator to help streamline the follow-up process. They are first implementing the algorithm at Penn Medicine hospitals and will then work to implement the algorithm at all hospitals across Philadelphia.
“The causes of maternal morbidity or mortality and disparities are so multifaceted,” Levine said. “To make a dent in the problem, you have to address it from all different angles.”
Banishing Biases that Perpetuate Racism in Health Care
Penn Medicine physicians are also leading the way in rooting out race-based medical measurements that perpetuate inequity.
Until 2021, anemia in pregnancy was diagnosed differently based on a patient’s race. The thinking had been that because Black women are more likely to be anemic (lacking a sufficient number of healthy red blood cells), pregnant Black patients needed to reach a lower red blood cell count than patients of other races to be diagnosed with and treated for anemia, Hamm said.
The race-based criteria were standardized by the American College of Obstetricians and Gynecologists (ACOG), and Penn Medicine followed that national guideline—until a Penn team’s research findings overturned it.
The race-based criteria for diagnosing anemia meant that Black patients were treated as though they were healthier than they actually were, Hamm said. By analyzing data from more than 1,000 pregnancies, Hamm found that pregnant Black patients at the Hospital of the University of Pennsylvania were much more likely to come to delivery with low hemoglobin, a protein contained in red blood cells. “People with lower hemoglobin are more likely to get a blood transfusion, which is associated with other morbidities like fatigue and postpartum depression,” Hamm said. “Likely this different definition of anemia was propagating disparities for Black women.”
In response to Hamm’s data—and as part of the maternal health overhaul—Penn Medicine stopped using ACOG’s race-based anemia guideline in 2020. Hamm and her team presented their data at a national maternal-fetal medicine conference in 2021, prompting ACOG to scrap its race-based criteria. “Now, anemia is defined nationally the same for everyone,” she said. Hamm’s team is currently working on a study with the health insurer Independence Blue Cross to determine how the guideline change has impacted Black women across Pennsylvania.

Pursuing Health Equity After Pregnancy
Penn Medicine’s efforts to address racial disparities in maternal health do not end in the hours and days after a baby is born. Penn Medicine’s efforts are system-wide and collaborative, geared toward having an impact at every time point, from prenatal care through childbirth and the first few weeks postpartum, and across a lifetime of care. Penn Medicine is also committed to sharing its successful efforts to improve health equity with other health care facilities, both locally across Philadelphia and wielding a national influence in the field.
“Let’s put equity first,” Howell has said. “Let’s not have it be the afterthought. Let it be the first thought.”







