It was early June 2020 when they first loaded their van with a pop-up tent, folding tables, masks, hand sanitizer, and a cooler full of testing chemicals.

A municipal parking lot known as “The Love Lot” became the site for multiple community services and programs in Kensington during the first year of the COVID-19 pandemic.
The world the Penn group now entered was one that McFadden and Abdulhay already knew — they’d both volunteered for years with Prevention Point, a nonprofit embedded in the community that is focused on empowerment, health, and safety for people who are affected by drug use and poverty. For his part, Davila was eager to jump in and help marginalized people, especially low-income Latinos who reminded him of where he’d come from.
The needs here are vast. Once an ordinary working-class neighborhood, over the last decade Kensington has become one of the largest hubs of the illicit opioid drug trade in the northeastern United States. The streets are home to hundreds of unhoused individuals, many of them in active substance use, many with medical comorbidities.
In tight quarters with few resources, this was a community at risk of being left behind and left out of newer forms of relief as the COVID-19 crisis unfolded. The Penn team reasoned that with very little money and a lot of dedication, they could make a difference by offering free tests. Along the way, with a short research survey, they hoped to gain some insight into how the pandemic was changing access to food, employment, and safe shelter — if people already at the edge of a cliff were in more danger of falling off, could the team learn how to save some of them?
And so the trio began driving to Kensington. Sometimes together, sometimes separately. At first every Tuesday, then three days each week when they got more funding. And they’ve kept going for nearly two years. Their story together makes up the Penn COVID TRACE project — for Testing, Resources, and Community Engagement.
“Whether it’s 110 degrees or 20 degrees, we are outside doing this every week,” McFadden says. “We were lucky because we got such a great team together. But also, the work feels very meaningful in a way that’s different from other roles that we have and other things that we do.”

Only Compassion and Help
“I’m 54 years old. I’m a mother and a grandmother and a wife. I’m an RN.” These are the first things Rose says when she’s asked to share her story one day late in the winter of 2022 while she waits in line for a COVID test in a tent outside of Prevention Point. She wants you to know that drug use doesn’t define her.

Rose used to work in home health care and as a certified eye bank technician. She would go to hospitals and funeral homes collecting corneal eye tissue for transplant. That’s not her life these days, though.
“When I was 33, I had gastric bypass and three other major abdominal surgeries. I was prescribed 700 Percocet 5s (5 mgs) in a year by the three different doctors that did the surgeries. I just kept on taking them, thinking I was in pain, but I probably wasn’t. I had a girlfriend say to me [years ago], ‘You’re not sick — that’s withdrawal.’ I realized I am addicted, totally.”
Her husband is, too — he got hooked on painkillers after a car accident 15 years ago that broke his neck. They currently live in a house in South Philly that has no electricity and no water. Her adult daughter also has a substance use disorder.
Rose comes to Kensington almost every day to get a meal. It takes an hour and a half to get here on the bus. Prevention Point usually serves food in the early afternoon, starting around 12:30.
Today, Roz Pichardo, the lead educator and community engagement coordinator, has made chili. Walking into the tent, before getting in line for her COVID test, Rose first stops at the Penn Medicine table to pick up the items being given out thanks to a grant from the city: a kit containing the drug Narcan to reverse overdoses and a warming bundle containing hand warmers and gloves tucked inside a knitted hat.
“I like this color for you!” McFadden calls out to Rose as she puts on the blue and yellow hat.
Rose adds the other items to her reusable shopping bag along with containers of food and a bunch of bananas Prevention Point has given her. Another bag she carries, a plastic one, has paper bags inside. They hold sterile syringes. Each week she collects dirty “works” around the neighborhood and turns them into the Prevention Point syringe service for sterile ones.
Rose has come to get tested about 10 times, she says. She had COVID about a month earlier and wants to confirm she’s still negative. She can’t go inside her methadone clinic if she’s positive for COVID. She explains that even though she’s on methadone to treat her drug use, she still does a couple bags of fentanyl a day. (“The methadone doesn’t block it. It’s like a super drug.”)
She says she got her COVID vaccine here last summer.
“It’s very convenient. Everybody’s friendly. They welcome you with open arms and treat you like a human being.”

Nabil Abdulhay, MPH, holds a sign for free COVID testing at the Love Lot, with Rachel McFadden, BSN, beside their tent.
The Love Lot
A coalition of programs and services started coming together at the Love Lot in the spring of 2020. Before COVID-19, Prevention Point ran clinics and syringe services five days per week and offered much more — case management, HIV testing and treatment, mail service for unhoused people — in their building, a former church in the shadow of the Market-Frankford El train running above Kensington Ave. With the pandemic, they suspended some services but brought as many as they could to a large municipal parking lot a few blocks away.
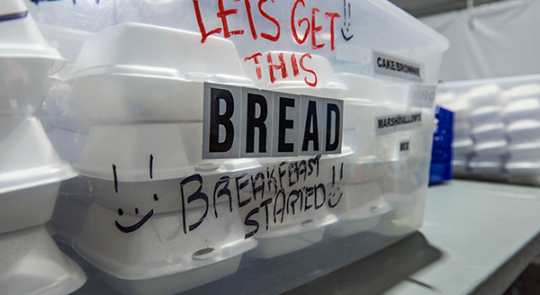
The Love Lot was one of three sites across the city where the “Step Up to the Plate” partnership, launched in the earliest days of the pandemic, brought together the City of Philadelphia, Prevention Point, and other community-embedded nonprofits, to offer free food for people facing the greatest needs.

Prevention Point looked for more ways to help with material needs — offering free clothing, changing stations to put on clean clothes, and assistance signing up to receive federal pandemic stimulus funds. And the Love Lot quickly became one of the only safe places for public life. Outside of mealtimes, there was the “Sunshine Café” serving tea, lemonade, and cocoa. A festive atmosphere was common, with musicians performing and artists running pop-up art-therapy workshops.
For more than a year, the Penn Medicine COVID TRACE project was one more player in this ensemble cast. It was built on the same premise of harm reduction that had been part of Prevention Point’s ethos for many years.
The Penn team offered COVID testing, for free, no appointments required, and, importantly, free of judgment — people could, and did, show up while in active substance use. In their research survey, the team asked participants a few basic questions about risk factors (in the first summer, almost 20 percent reported they’d spent time with someone with COVID), and about resources like jobs, housing, and food, in order to track any correlations with positive tests. About 30 percent of participants were living on the street, and another 7 percent in shelters. And the Penn team shared information about staying safe, whether from COVID or from overdoses, along with protective tools including masks, hand sanitizer, and Narcan.
The judgment-free zone was welcoming to people who might not seek care in a traditional health clinic.
“I truly believe interfacing with health care clinicians in that kind of harm reduction framework can start rebuilding the damaged, distrustful relationship between health care and people who use drugs,” McFadden says. “That’s kind of a big thing.”

Grassroots to Growing Up
“I’m going to be honest, it was like chaos, it was just get through it,” Abdulhay recalls of the first summer of testing. “Just do whatever you can do.”
As the nurse, McFadden did all the swabbing for samples to run PCR tests — aided by a slew of dedicated nursing students from the Community College of Philadelphia, and their clinical instructor, Matthew Liccketto, RN, also a nurse at Penn Medicine, who volunteered to help.

“When it gets really busy, we need to form a line, keep things orderly,” Abdulhay adds — it’s part of his job to be the logistics ace. “That’s a challenge, and that’s where also where Prevention Point steps up. Roz Pichardo, she’s extraordinary and can very quickly turn a messy situation around.”
That whole first year, at the Love Lot every Tuesday, the team used a totally analog system for their research questionnaire and testing materials. “Everything was labeled four times for redundancy and everything was just label on label on label on handwritten surveys,” Abdulhay says.
That first summer turned to winter, and the trio still came every Tuesday. They had hand warmers but no other source of heat. McFadden’s fingers turned blue as she tried to draw blood samples for an antibody-testing part of the study that was later discontinued.
Trying to fill out the paper surveys, Davila recalls, he had to hold the pen in his armpit to keep the ink from freezing.
This type of street-level outreach wasn’t even close to Davila’s specialty. After freezing on Tuesdays at the Love Lot, he spent all day every Wednesday in his lab running the PCR tests to turn around results in 24 hours. Every piece of the test was prepared in his lab — all the solutions, everything in each tube.
Then, in May 2021, the Philadelphia Department of Public Health awarded the team a grant of nearly $500,000 to expand their operation. Abdulhay found the time to dust off some old iPads and digitize their surveys. Bolstered by a new staff of paid assistants, the team could offer free testing three days every week. The city grant provided rapid antigen tests so that community members could get their results on the spot in 15 minutes, while they could still also opt into taking the Penn PCR test and research survey. If they chose the latter, they could earn a $5 Wawa gift card. Some took both tests — and, often, supplies for both ran out early in the day.

Antonio Davila, PhD, stepped outside of his comfort zone as a laboratory scientist through his work with COVID TRACE.
Assembling a Dream Team
“As a team we were always able to bring different things to the table,” Abdulhay says. “Tony runs a lab that can run all these samples. Rachel is the person who can talk to anybody under any circumstances, and I’m the guy that runs all the background stuff and can set up all the when and where.”
Remarkably, the three of them barely knew each other before the pandemic.
To start, in those early days when COVID tests were scarce, Davila got curious and a tiny bit rebellious. He kept coming to the lab when it was supposed to be shut down and he learned what he needed to run his own PCR test for the SARS-CoV-2 virus.
Abdulhay had seen his own work on Penn’s Mobile CPR project shut down — it was no longer safe to gather groups for hands-on CPR training to help bystanders save lives from cardiac arrest. In the early spring of 2020, he seized the opportunity to staff a research study looking at whether the malaria drug hydroxychloroquine could prevent COVID infection in health care workers. (They ultimately found the answer was no — it wasn’t any more effective than a placebo.) One of the study’s lead investigators, Benjamin Abella, MD, MPhil, had overseen Abdulhay’s CPR work in his role as director of Penn’s Center for Resuscitation Science.
It was Abella who brought them all together. He’d also worked closely with Davila as medical director of PARC; that group did studies related to traumatic emergency conditions, ranging from blood clotting to brain injury. And Abella had worked side by side with McFadden caring for patients in the Emergency Department at HUP. He knew that both she and Abdulhay had volunteered with the syringe services and wound clinic at Prevention Point before. And so they all came together.
“The common theme for all four of us is we just really care about the community and want to stay involved,” Abella says.
“One of the most commonly stated values that I put on the table is I want to be a research team that has dirt under its fingernails. I don’t want to just live in the ivory tower. You know, learning stuff is nice, but putting that knowledge and skillset to work in the community is even nicer.”

Mama Sunshine
“People got to sit down and chill with us,” says Roz Pichardo. “This was like the only space that was okay during COVID.” Pichardo works both at Temple University Hospital, where she is an advocate for trauma victims, and at Prevention Point, where she works in education and community engagement.
Here, she’s known as Mama Sunshine because she calls all the participants “Sunshine.” It’s an endearing and universal term that everyone responds to, unlike the dehumanizing names too many people call them — like addicts, or zombies.
She’s grateful for the Penn team coming to give free testing in Kensington.
“It’s been helpful, not only for the participants, but it’s been helpful for us as essential workers,” she says. “We don’t have time to go downtown to get tested.”
Pichardo, who lives in Kensington herself, has had COVID four times and survived a bout in the ICU the second time, before the vaccines came out. She has helped many more in her community to survive their other epidemic. In a pocket-sized black Bible, she counts them: Using Narcan, she has reversed 924 overdoses since 2018.
Since funding for Step Up to the Plate ended at the end of 2021, free meals from Prevention Point are no longer a guarantee. Yet Pichardo has been committed to making sure food still flows in, including grocery donations from another local nonprofit, SHARE Food. Often, she personally cooks and packages huge quantities of chili or macaroni and cheese.

Prevention Point runs a syringe exchange five days per week, year-round. It is a form of harm reduction, offering people who use drugs a way to do so with less risk of infection, and helping to build trust to connect with other forms of support.
Where They Are
In the fall of 2021, a few things changed. Prevention Point and their partners shifted their meal distribution from the Love Lot to Prevention Point’s own headquarters. A large tent with clear plastic flaps sits in a parking lot adjacent to the building, more sheltered than before. And for the second COVID winter, they had heaters.
The renewal of city funding for Penn’s COVID testing program made it possible to add testing once a week in West Philadelphia in partnership with the People’s Emergency Center.
Demand for testing in Kensington has fluctuated over time — rising during the delta and omicron waves, declining in between. Despite the Penn team’s earlier concerns of potentially high COVID rates in this community, the testing program didn’t bear that out; they were reaching a group of people who avoided this disease, perhaps because most can’t afford to take public transportation and don’t congregate indoors or eat in restaurants. But the need for connection and support has been constant, and it’s central to Prevention Point’s role to be there with partners, including Penn Medicine, at their side, to reduce harm for people in the depths of a powerful substance use disorder.
“The syringe services program is the classic example of harm reduction,” Prevention Point’s Disch explains, “because we’re not telling people you need to stop using drugs, we’re saying we understand you’re using drugs, and you still deserve to stay safe and healthy. If you use an unsterile syringe, you’re more likely to develop infections. We’ve seen that if you can meet someone with an immediate need like a sterile syringe and they start to trust you, maybe they’ll be open to more services like testing for HIV or Hep C, or treatment.”
It’s a lesson that some more empathetic emergency medicine clinicians like McFadden and Abella also bring to their care of unhoused individuals in the hospital on a regular basis, too — though stigma against them and those with substance use disorder is also still common.
“These are folks who the world does not treat well,” Abella reflects. “The ability to bring them a sandwich, treat them with dignity, talk to them a little bit, and if they need a place to sleep for an hour, let them sleep for an hour before we send them out, is an act of kindness that feels like a really important thing because they don’t get this very often in their existence, unfortunately.”


Where They’re Going
For some among the trio Abella brought together, who have shown up every week in Kensington for nearly two years, the experience has been transformative. Yet they are all a little unsure about what lies ahead, as the city’s funding for their testing program was slated to run out after this May.
McFadden is connected to this community no matter what; she’ll keep working at the front lines in HUP’s Emergency Department and volunteering with Prevention Point as much as she can.
At the Love Lot, Davila was pushed out of his comfort zone in the lab. He had wanted to help, but he thought his role was lending his hand to a research study. Face to face with real people in dire straits, he had a realization: “We weren’t really a research project. We were a service.”
From that point forward Davila’s priority wasn’t the data they’d collect, but what they could collectively do to help people — from testing to warm clothing. Meanwhile, his research lab is back up and running now after the early COVID closure, but he’s not just returning to his old projects.

“My life has completely changed since this started,” says Davila, who’s also a faculty member in Penn’s School of Nursing. He’s envisioning public health research focused on trauma; he wants to measure how the body responds to exposure to community violence, and how that impacts healing from injury. And he’s thinking about, beyond the lab work, how he will collaborate with community partners and spend time with the people affected by that trauma.
Abdulhay, who completed his master’s in public health degree at Penn this spring, is still committed to the lifesaving mission of community CPR training that was once his primary job — and may be again, one of these days.
“I’d really love to return to our core CPR work and cardiovascular work,” Abella agrees. “It’s like the farmer-soldier, though. If you have to go fight the war, you fight the war and you just keep dreaming of getting back to the farm. You know, when the war’s over, I’d love to get back to what we did before COVID. But if there’s still work to be done, we’re here for it.”
















